When families are told that their baby may not survive pregnancy or life after birth, the news can feel overwhelming and impossible to process. At Helen & Douglas House, families don’t have to face this journey alone. Michaela, our Advanced Clinical Practitioner for Perinatal Palliative Care, alongside the wider team is there to walk alongside them, offering care, guidance and compassion at one of the hardest times imaginable. Michaela has worked as a midwife for 16 years in delivery suite and has cared for women following stillbirth.
Her role was born out of a decade of experience delivering a Perinatal Palliative Care Pathway. Previously, this pathway was more reactive than proactive – medical teams had to fit this vital work around other responsibilities, which limited early identification and timely support. Michaela’s dedicated post marks a significant shift, enabling earlier engagement with families during pregnancy and after birth when their baby has a serious or life-limiting condition. This is often from around 20 weeks of pregnancy, rather than waiting until after delivery.
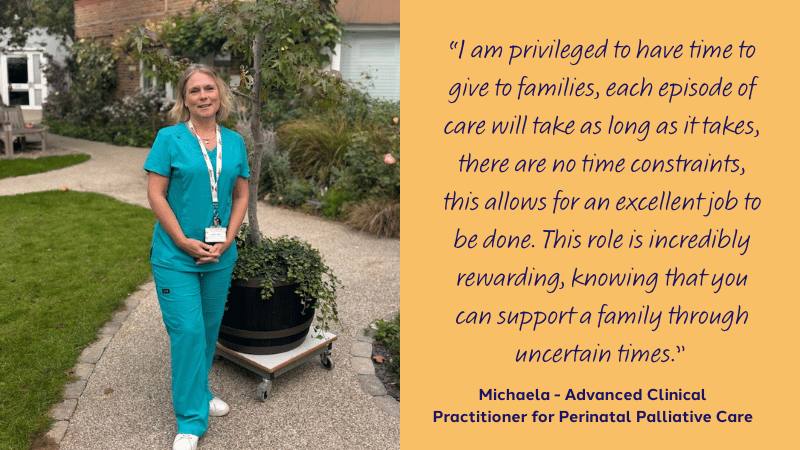
Michaela’s role
Michaela’s role bridges hospital and hospice care, ensuring families are supported at every step. She works closely with the Fetal Medicine Unit, neonatal teams, obstetricians, midwives, and the wider multi-disciplinary team to make sure no family falls through the gaps.
Her work includes:
- Meeting families during pregnancy following difficult or uncertain diagnoses (such as Edwards syndrome or Patau syndrome) and complex cardiac conditions.
- Helping parents explore their options, parallel-plan, plan for birth as well as Advanced Care Planning that reflects their wishes.
- Supporting babies and families on the neonatal unit – not just at end-of-life, but throughout complex and uncertain journeys.
- Advocating for early referrals and raising awareness that palliative care isn’t just about end-of-life, but about living well, however short life may be.
By connecting hospital and hospice teams, Michaela helps families feel less isolated and gives professionals the confidence to offer palliative support sooner.
A week in Michaela’s life
Michaela divides her time between John Radcliffe Hospital in Oxford and Helen & Douglas House. No two days look the same, but her focus is always on being there for families when they need it most.
“One day I might be meeting a mum after a scan to talk through her baby’s diagnosis, the next I’ll be at the hospice helping our nursing team support a child coming in for a stay.”
At the hospital she joins ward rounds, attends multi-disciplinary meetings, and meets parents in the Fetal Medicine Unit, often over a quiet coffee away from the ward. She works closely with neonatal staff, midwives, and obstetricians to co-ordinate care and advocate for families. She also supports families during the end of life and memory making.
At the hospice she helps with admissions and discharges, prescribes medication, supports the nursing team, and plans care for children and babies with complex needs.
Following delivery, she provides compassionate support at home or in the hospice for up to six weeks, offering emotional care, practical guidance, and signposting to our in-house bereavement service for families who wish to access further support.
Alongside her incredible work supporting families across hospital, hospice, and home settings, Michaela also attends and speaks at national forums and has been featured on the All4Maternity podcast, Midwifery: Love, Life and Learning. You can listen to the episode here.
The impact
Michaela’s presence makes an enormous difference to families by:
- Offering a safe space to talk openly about fears, hopes, and choices.
- Ensuring parents feel less alone during an uncertain pregnancy.
- Helping families plan for the future with dignity and compassion.
- Bridging care between hospital and hospice, so families don’t feel like they are starting over at each stage of the journey.
Her role also helps change perceptions among healthcare professionals. By being a visible presence on the neonatal unit, Michaela reminds colleagues that palliative care is about more than end-of-life.
“It is so important to have a presence within the units so the staff remember the hospice as an organisation that can offer daily support, not just for end-of-life or post-death. Encouraging staff to come and visit us to see what we are all about, this will then help them to describe the beautiful happy space we have here, not the gloomy sad place it is often perceived to be”.
Challenges and hopes for the future
Many people still see hospices only in the context of death and dying. Michaela is working to change that narrative by inviting staff and families to see Helen & Douglas House for what it truly is – a warm, supportive, and happy space.
Looking ahead, Michaela hopes to:
- Expand the service to Swindon and Milton Keynes.
- Increase the number of antenatal and neonatal referrals, ensuring support starts earlier in families’ journeys.
- Develop a monthly mother-and-baby group to provide peer support and connection.
Being part of the team
Michaela says one of the best things about her role is the sense of belonging at Helen & Douglas House.
“I love the challenges of setting up a new and worthwhile service, and the knowledge that we can provide excellent care for our families. Being part of the care team feels like being part of a family – we all support each other, as well as the children and families we care for.”

Why Michaela’s role matters
During Baby Loss Awareness Month, we are reminded that behind every diagnosis is a family navigating heartbreak, uncertainty, and hope. Michaela’s role ensures that from the very beginning of their journey, families never have to walk it alone.
An example of compassionate support
An example of the perinatal role in action came through our support of a family referred to Helen & Douglas House during pregnancy who after learning their baby was unlikely to survive, experienced the devastating loss of their son at 26 weeks’ gestation. Michaela worked closely with them to create a personalised birth plan that honoured their wishes and gave them space to grieve. From facilitating memory-making to a peaceful stay at the hospice, every detail was guided by compassion and collaboration. The family spent 48 hours with their baby in the Little Room at Helen & Douglas House in a calm, supportive environment, creating lasting memories through photos, keepsakes, and quiet time together. Our care continued beyond their stay, with regular follow-up and emotional support. The family expressed deep gratitude for the care and support they received, both during their time at Helen & Douglas House and in the weeks that followed. They felt listened to, respected, and cared for at every stage.

Michaela’s work is so important – not just in Oxford, but as part of a national movement towards earlier, more compassionate perinatal palliative care. Her dedication is helping families feel seen, heard, and supported when it matters most.
