Clinical Research
Helen & Douglas House has been involved in a number of research projects over our 40+ year history.
Helen & Douglas House has been involved in a number of research projects over our 40+ year history. These have focused on understanding and improving patient and family experience of receiving care, including pain management, support for children with feeding tubes, and spiritual care needs. We believe that our patients have an equal right to care based on the experience of their own peers. This is likely to be safer and to better meet their individual needs.
Using co-production to improve patient experience | Q Exchange
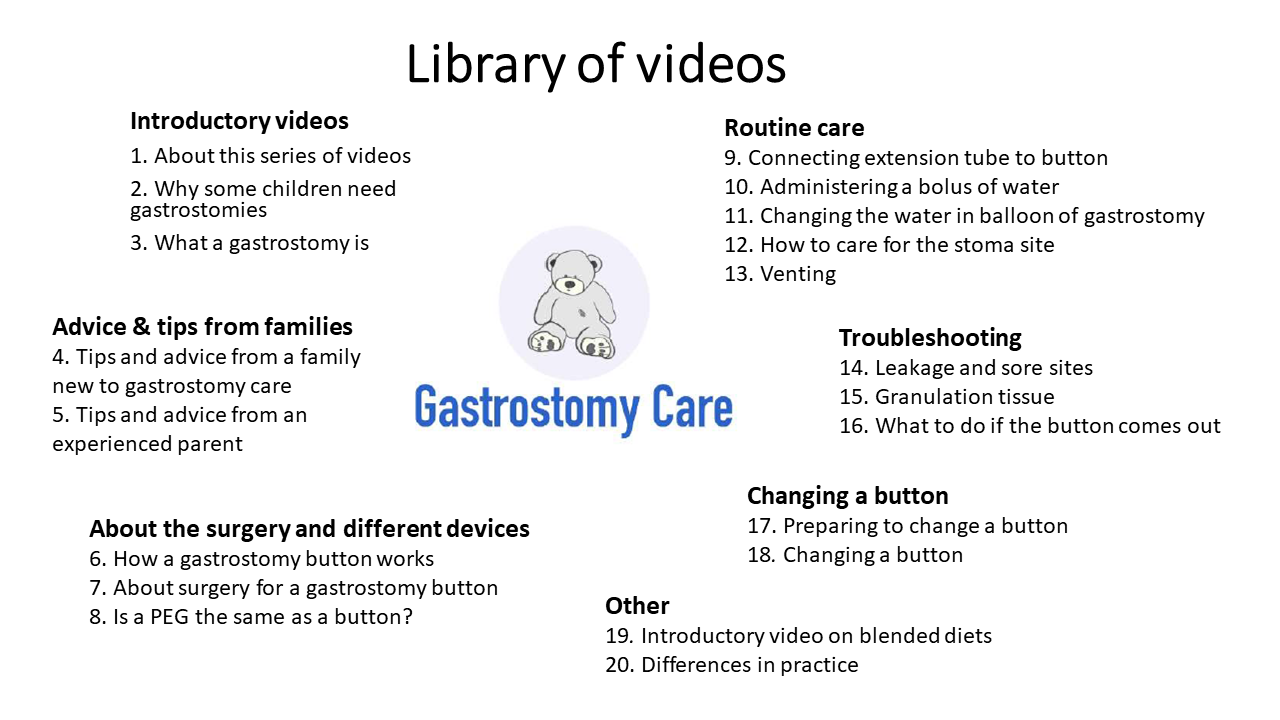
Many families now perform specialist medical procedures at home. Families need appropriate training and support to do this. The aim of this study was to evaluate a library of videos, coproduced with parents and healthcare professionals, to support and educate families caring for a child with a gastrostomy. This work is in partnership with OUHT and Oxford University. This research was was also supported by families from Helen & Douglas House and our team of doctors. A team of parent representatives, researchers and healthcare professionals from the hospital and community have been involved in creating these videos. Earlier in the project we did a survey with 150 families to understand their experiences of training and what types of videos would be most helpful. You may have taken part in this. Key things we learnt from the survey:
- Families wanted both healthcare professionals and parents to feature and that they wanted some videos to be filmed at home and to show "real life".
- Families wanted help with managing common problems.
- Families valued advice and tips from more experienced families.
 You can read more about the research itself, the evaluations and watch the videos themselves from the links on the right.
Read more
You can read more about the research itself, the evaluations and watch the videos themselves from the links on the right.
Read moreThe CoPPAR Network
Addressing the current gap in quality research in paediatric palliative care requires a shared and collaborative response between the academic and paediatric palliative care sector. The aim is to provide a UK wide Collaborative Paediatric Palliative Care network that will foster and assist the sectors to work alongside one another to deliver national high-quality research studies. The vision of CoPPAR is that it will become the single point of information for all pediatric palliative care research across the UK that can be accessed by researchers, clinicians, parents and young people, and policy makers to enable more effective and efficient delivery of research in this sector. Read more
Medical Mediation Foundation | The True Colours Trust
Difficult decisions are often faced in clinical settings, especially where children are being treated. Sadly, in some cases, differing opinions about care or treatment can result in conflict between families and the clinicians treating their children. These conflicts can have a deep and long-lasting impact on all parties. True Colours is delighted to be working with the Medical Mediation Foundation on an exciting initiative to embed the use of conflict management and mediation skills within clinical teams. This three-year project sees MMF working with three specialist UK hospitals to train staff in how to recognise and manage potential conflicts between families and health professionals. The hospitals involved are Leeds Children’s Hospital, Newcastle’s Great Northern Children’s Hospital and the Oxford Children’s Hospital/ Helen & Douglas House Hospice for Children. Since April 2021, MMF have delivered 90 training session to 480 health professionals. Of these, 95% said the training was "very relevant". Our doctors and care staff look at children's conditions and treatments as a whole, taking into account what is important for the child and the family so we can give them the best care. Read more
Children’s Palliative Care Outcome Scale (C-POS)
C-POS aims to develop, validate, and implement a person- and family-centred outcome measure that can be used by CYP and their families affected by LLLTC. The study will identify CYP, family, professional and commissioner priority concerns and outcomes in paediatric palliative care, which will be used to inform item generation and initial measure development. The C-POS will be the first fully validated children and family centred outcome measure for use in paediatric palliative care. The study brings together families, researchers, health and social care professionals and champions children’s voices in the research, rather than relying on proxy data. The tool will be implemented into routine clinical practice which if used regularly to measure and document change in patient’s status, can inform and improve care for children and young people with life-limiting and life-threatening illnesses. Read more
The BEACON Study – Development and validation of a paediatric breakthrough pain assessment tool
This is an upcoming research study examining the best way to measure breakthrough pain in children already taking regular pain medicine. Breakthrough pain is the discomfort experienced when the symptom is temporarily worse than the existing medication can deal with and needs rapid treatment with top-up medication. Interviews will take place with young people, and their parents / carers, leading to the development of a tool, which will then be reviewed by patients, parents and healthcare professionals. The work involves several other specialist centres and is funded by Great Ormond Street Hospital Charity, and took place over an 18 month period (2022-2024). Outcomes: Despite all efforts made, there is still no consensus on the definition of breakthrough pain. A compromise is needed on the vocabulary of breakthrough pain in order to collect reliable incidence and prevalence data. Read more
Undertaking doctoral research with children and young people with life-limiting or life-threatening conditions
Research project from Together for Short Lives (TfSL) and the Association of Paediatric Palliative Medicine (APPM) for identifying ways to support and develop those undertaking or considering doctoral studies concerning children and young people with life-limiting and life-threatening conditions and those who provide care and support to them. Read more
Analysis of paediatric long-term ventilation incidents in the community.
The aim of this research was to describe the nature and causes of reported patient safety incidents relating to care in the community for children dependent on long-term ventilation with the further aim of improving safety. Read more
Communication with children and adolescents about the diagnosis of their own life-threatening condition
When a child is diagnosed with a life-threatening condition, one of the most challenging tasks facing health-care professionals is how to communicate this to the child, and to their parents or caregivers. This paper reviews the effect of communication on children's emotional, behavioural, and social functioning, as well as treatment adherence, disease progression, and wider family relationships. Read more
Barriers and facilitators experienced by patients, carers and healthcare professionals when managing symptoms in infants, children and young people at end-of-life: a mixed methods systematic review protocol
This review will inform understanding of symptom management in ICYP at end-of-life. Read more
Towards developing an ethical framework for decision making in long-term ventilation in children
The use of long-term ventilation (LTV) in children is growing in the UK and worldwide. This reflects the improvement in technology to provide LTV, the growing number of indications in which it can be successfully delivered and the acceptability of LTV to families and children. This article discusses the various considerations to be made when deciding to initiate or continue LTV, describes the process that should be followed, as decided by a consensus of experienced physicians, and outlines the options available for resolution of conflict around LTV decision making. Read more
Fifteen-minute consultation: perinatal palliative care
Perinatal palliative medicine is an emerging subspecialty within paediatric palliative medicine, neonatal medicine, fetal medicine and obstetrics. This paper defines and describes one model for providing perinatal palliative care, drawing on the personal and professional experience of the authors. Read more
Promoting high quality research with life-limited children and their families: Establishment of a joint research group between Together for Short Lives and the Association for Paediatric Palliative Medicine
Together for Short Lives-Asssociation for Paediatric Palliative Medicine [TfSL-APPM] research group was formed in recognition of the challenges in research with life limited children and their families and in the hope that by coming together – researchers and clinicians for a number of disciplines- we could contribute to the solutions. Read more
Fifteen-minute consultation: Developing an advance care plan in partnership with the child and family
An advance care plan (ACP) is the record of a discussion between an individual (where possible), their professional care givers and those close to them about their future care. When performed well, the process provides all those involved with the opportunity to talk honestly about the future allowing children and their families to retain autonomy and to influence how they are looked after. The multidisciplinary writing team, share their experiences, in the context of recent national guidance, on the use of ACPs. Read more
Barriers to the use of buccal and intranasal fentanyl for breakthrough pain in paediatric palliative care: an exploratory survey
The aim of this survey was to investigate current off-label prescribing of fentanyl for breakthrough pain relief in paediatric palliative care and to ascertain any barriers to use. Read more
Palliative medicines for children – a new frontier in paediatric research
This paper seeks to highlight from a UK perspective the current lack of a research evidence base in paediatric palliative care that has resulted in a paucity of available medicines with appropriate formulations (strength and dosage form) to provide symptom management for children with life-limiting illnesses Read more
Blended foods for tube-fed children: a safe and realistic option? A rapid review of the evidence
With the growing number of children and young people with complex care needs or life-limiting conditions, alternative routes for nutrition have been established (such as gastrostomy feeding). Read more
Fifteen minute consultation: Practical pain management in paediatric palliative care
Understanding the child's underlying condition, possible causes of pain and their preferred mode of communication are important to the delivery of holistic care. This article aims to explore this. Read more
End of life care for infants, children and young people with life limiting conditions: summary of NICE guidance
Children and young people can have a wide range of life limiting conditions and may sometimes live with such conditions for many years. This guideline recommends that end of life care be managed as a long term process that begins at the time of diagnosis of a life limiting condition and entails planning for the future. Read more
The Spectrum of Children’s Palliative Care Needs: a classification framework for children with life-limiting or life-threatening conditions
This paper examined the potential of a new classification framework, The Spectrum of Children's Palliative Care Needs, to facilitate identification of children with palliative care needs for the purposes of minimum data set collection and population needs assessment. Read more
The characteristics and experiences of anticipatory mourning in caregivers of teenagers and young adults
This article reports a systematic review of literature undertaken to identify characteristics and experiences of anticipatory mourning in caregivers of teenagers and young adults with life-limiting or life-threatening conditions. This review focused on six studies that met inclusion criteria and reported characteristics of anticipatory mourning in caregivers of teenagers and young adults. Characteristics and experiences were sorted into four main themes: symptoms; a sense of loss; caregiver behaviour; and the unique experience of caring for, or losing, a teenager or young adult. The review suggests that there are characteristics and experiences of anticipatory mourning that are unique to caregivers of this age group. Read more
Realistic nurse-led policy implementation, optimization and evaluation: novel methodological exemplar
Health policies are increasingly complex, involve multiple Government departments and frequently fail to translate into better patient outcomes. Realist methods have not yet been adapted for policy implementation. The aim of this research was to report the first large-scale realistic nurse-led implementation, optimization and evaluation of a complex children's continuing-care policy. Read more
Journey from paediatric intensive care to palliative care
Approximately two-thirds of patients who die in the pediatric intensive care unit (PICU) do so following withdrawal of intensive care treatment. Most often when intensive care treatment is withdrawn, the child remains in the PICU for end-of-life care. This study aimed to examine the process of referral over a 6-year period of children from a PICU to children's hospices for end-of-life care. Read more
Learning from paediatric palliative care: lessons for adult practice
A research study into the learnings from palliative paediatric care and the transition from child to adult practice. Read more
Total pain: a reflective case study addressing the experience of a terminally ill adolescent.
The research demonstrates how the care delivered by local services was informed by UK strategies for palliative and oncological care of young people. Read more
How and when to refer a child for specialist paediatric palliative care
Specialist paediatric palliative care is a relatively new area of paediatrics, and the interface with other disciplines can occasionally pose challenges for referrers due to lack of information about the diverse services available. Although services vary on a regional basis, there are common principles which may be used to guide and support referrals. This research aimed to clarify the role of specialist paediatric palliative care, identify who should be eligible for such care, describe the services available (including those from children's hospices) and provide a tool for assessing some of the most challenging referrals. Read more
A study into the educational needs of children’s hospice doctors: a descriptive quantitative and qualitative survey
This research study was conducted to identify and explore the educational needs of children's hospice doctors in England. Read more
A survey of signs, symptoms and symptom control in 30 terminally ill children
The notes of 30 terminally ill children with various diagnoses were searched for reports of symptoms that had occurred during their last month of life. All had stayed at Helen House, a hospice for children, for part or all of that time. The results were analysed for symptom frequency and resistance to treatment. Read more
Medical and nursing problems of children with neurodegenerative disease.
Little is written on the management of problems encountered by children with neurodegenerative disease. Whilst the conditions are individually rare, as a group of diseases they pose a considerable burden on the child, the family and the community. This study describes the 127 children with neurodegenerative disease who were admitted to Helen House, a hospice for children, from the time of opening in November 1982 until the end of 1993. Read more
Helen & Douglas House – a hospice for children: analysis of the first year
Helen & Douglas House hospice for terminally ill babies and children opened in November 1982. This article looks at the first year of the hospice and how it helped many children in the community. Read more
Coproducing a library of videos to support families caring for children with gastrostomies: A mixed-methods evaluation with family carers and clinicians.
Many families now perform specialist medical procedures at home. Families need appropriate training and support to do this. Similar coproduced educational materials are needed to support families who perform other medical procedures at home. Read more
Pain assessment tools in paediatric palliative care: A systematic review of psychometric properties and recommendations for clinical practice.
Assessing pain in infants, children and young people with life-limiting conditions remains a challenge due to diverse patient conditions, types of pain and often a reduced ability or inability of patients to communicate verbally. The aim of this review was to systematically identify pain assessment tools that are currently used in paediatric palliative care and examine their psychometric properties and feasibility and make recommendations for clinical practice. Read more
The challenges of caring for children who require complex medical care at home: ‘The go between for everyone is the parent and as the parent that’s an awful lot of responsibility’.
Increasing numbers of children with complex health-care needs are cared for at home by their family. The aim of this qualitative study was to explore the challenges experienced by families caring for children who need complex medical care at home. Read more
Training and support for caring for a child’s gastrostomy: a survey with family carers.
The aim of this study was to explore family carers’ experiences of training and ongoing support for caring for their child’s gastrostomy, and to get their views on how this could be improved. Read more
Managing and sharing research data in children’s palliative care: Risks, benefits and imponderables.
Joint research with Together for Short Lives and Association of Paediatric Palliative Medicine into the managing and sharing of research data in children’s palliative care. Read more
A Systematic Review of Measures of Breakthrough Pain and Their Psychometric Properties.
Breakthrough pain (BTP) is common in cancer and other conditions yet there is a lack of validated BTP measurement tools. The aim of the review was to identify all tools assessing or characterising BTP in patients of any age with any condition, and to critically appraise their psychometric properties. Read more
Development of a research-based classification of approaches to paediatric palliative medicine service provision within children’s and young adults’ hospices: A mixed methods study.
Globally, pioneers in children’s palliative care influenced this speciality’s development through individual initiatives leading to diverse models of care. Children’s and young adults’ hospices have now been established around the world. However, service provision varies widely leading to inequities both within countries and internationally. The aim of this study was to describe and classify existing approaches to paediatric palliative medicine in children’s and young adults’ hospices across the UK. Read more
Healthcare Professionals’ Experiences of the Barriers and Facilitators to Pediatric Pain Management in the Community at End-of-Life: A Qualitative Interview Study.
Inadequate pain management in community pediatric palliative care is common. Evidence to inform improved pain management in this population is limited. The aim of the study was to explore the barriers and facilitators to pediatric community-based pain management for infants, children and young people at end-of-life as perceived by healthcare professionals. Read more
Diamorphine pharmacokinetics and conversion factor estimates for intranasal diamorphine in paediatric breathrough pain: systematic review
Intranasal diamorphine is a potential treatment for breakthrough pain but few paediatric data are available to assist dose estimation. The aim of the review was to determine an intranasal diamorphine dose in children through an understanding of pharmacokinetics. Read more
A mixed-methods systematic review and meta-analysis of barriers and fascilitators to paediatric symptom management at end of life
Symptom management for infants, children and young people at end of life is complex and challenging due to the range of conditions and differing care needs of individuals of different ages. The aim of the review was to investigate the barriers and facilitators experienced by patients, carers and healthcare professionals managing symptoms in infants, children and young people at end of life. Read more
A protocol for a systematic review and meta-analysis to identify measures of breakthrough pain and evaluate their psychometric properties
Breakthrough pain is common in children and adults with cancer and other conditions, including those approaching end-of-life, although it is often poorly managed, possibly partly due to a lack of validated assessment tools. This review aims to (1) identify all available instruments measuring breakthrough pain in infants, children, adolescents or adults and (2) critically appraise, compare and summarise the quality of the psychometric properties of the identified instruments using COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) criteria. Read more
Healthcare professionals’ views of the use of oral morphine and transmucosal diamorphine in the management of paediatric breakthrough pain and the feasibility of a randomised controlled trial: A focus group study (DIPPER)
Oral morphine is frequently used for breakthrough pain but the oral route is not always available and absorption is slow. The aim of this study was to explore the perspectives of healthcare professionals in the UK caring for children with life-limiting conditions concerning the assessment and management of breakthrough pain; prescribing and administration of transmucosal diamorphine compared with oral morphine; and the feasibility of a comparative clinical trial. Read more
Oral morphine versus transmucosal diamorphone for breakthrough pain in children: methods and outcomes: UK (DIPPER study) consensus
No randomised controlled trials have been conducted for breakthrough pain in paediatric palliative care and there are currently no standardised outcome measures. The DIPPER study aims to establish the feasibility of conducting a prospective randomised controlled trial comparing oral and transmucosal administration of opioids for breakthrough pain. The aim of the current study was to achieve consensus on design aspects for a small-scale prospective study to inform a future randomised controlled trial of oral morphine, the current first-line treatment, versus transmucosal diamorphine. Read more
Transmucosal drug administration as an alternative route in palliative and end-of-life care during the COVID-19 pandemic
The Coronavirus disease 2019 (COVID-19) pandemic has led to a surge in need for alternative routes of administration of drugs for end of life and palliative care, particularly in community settings. Transmucosal routes include intranasal, buccal, sublingual and rectal. They are non-invasive routes for systemic drug delivery with the possibility of self-administration, or administration by family caregivers. The aim of this research was to provide insights into using transmucosal drug delivery to bring about the best possible symptom management for patients at the end of life, and to inspire scientists to develop new delivery systems to provide effective symptom management for this group of patients. Read more
Orodispersible and transmucosal alternative medications for symptom control in adults
Paediatric palliative care makes frequent use of orodispersible and transmucosal drug delivery routes. The limited published experience of this practice suggests that it enables the delivery of needle-free symptom relief, with the potential to train family carers to administer anticipatory medications without reliance on trained health professionals. The aim of this research was to identify orodispersible and potential transmucosal alternatives that may be used in adults in the event of a patient having no oral or intravenous route and no access to subcutaneous injections. Read more
The SPARK Project
The SPARK Project examines the best way to deliver pastoral, spiritual and religious care to children with life limiting illnesses and their families. Helen & Douglas House were involved in recruiting families pre- and post-bereavement to take part, as well as supporting focus groups. At the moment, we know very little about how to meet the pastoral, spiritual and religious needs of children and young people diagnosed with a life-threatening or life-shortening condition, and their parents. This study was done over 3 years from August 2020, to March 2023. The study involved focus groups and interviews with care givers, children and healthcare professionals to better understand their practices, needs and views.The aim of this study was to gather evidence the NHS and children's hospices can use to guide how they meet these needs, including the role of chaplaincy services (sometimes called pastoral and spiritual care services). It will also explore how chaplaincy services can support clinical and care teams involved in the care of these children and young people. The conclusion from this study was that having a life-shortening or life-threatening conditions brings multiple threats to the spiritual wellbeing and lived experiences of children and young people and their families. It demonstrated the need for more training in this area particularly in the NHS. From this study, it's recognised that spirituality and spiritual care needs to be part of a child's care pathway. Read more